How We Work
Frequently Asked Questions about Bow Leg Correction
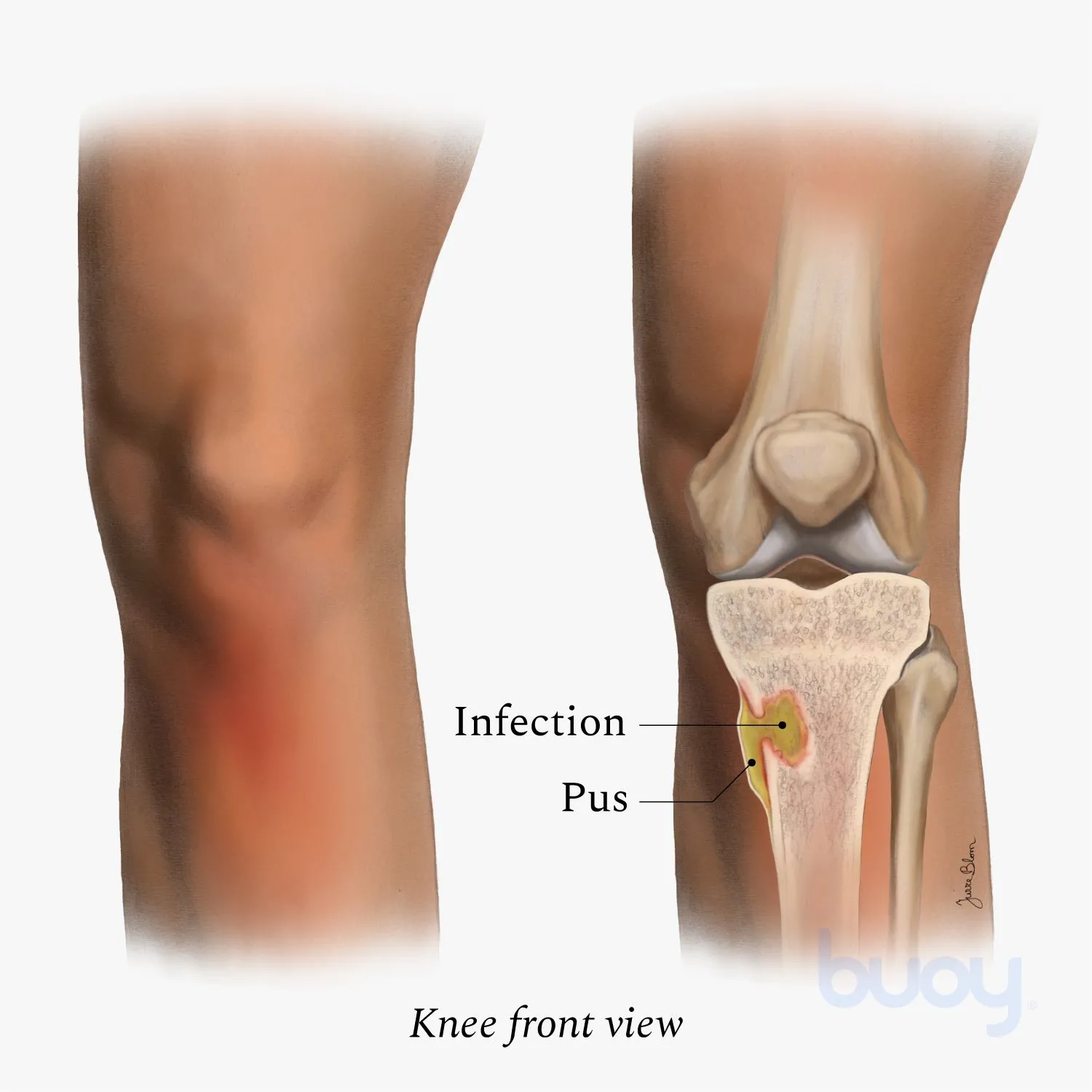
What causes bone infections?
Bone infections typically result from bacterial invasion through open wounds, surgical sites, or bloodstream spread from other infected areas in the body. Common risk factors include diabetes, compromised immune system, and previous bone trauma.
How serious is a bone infection?
Bone infections are serious medical conditions that can lead to permanent bone damage, chronic pain, and life-threatening complications if left untreated. Early diagnosis and treatment are crucial for optimal outcomes.
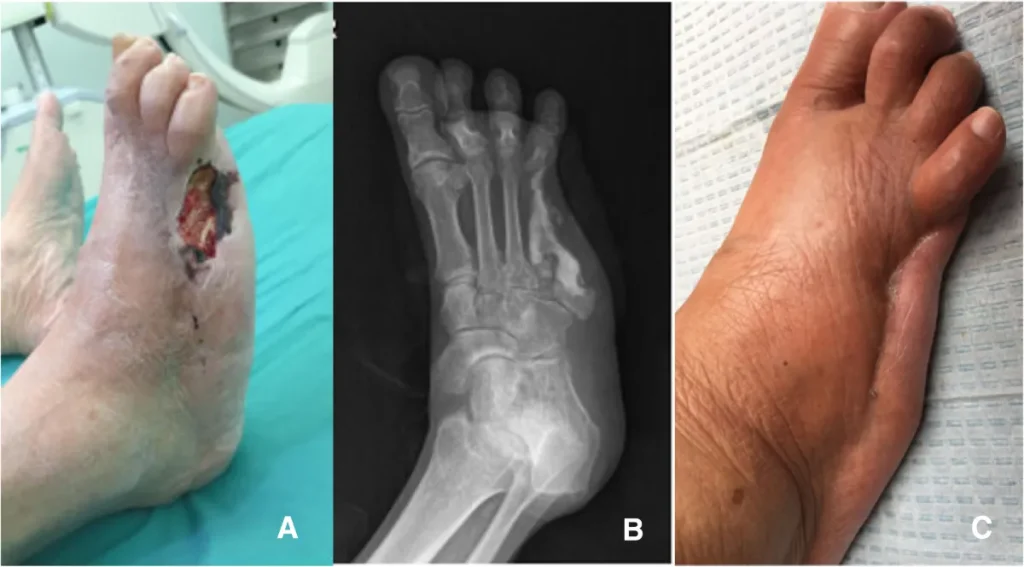
What is the success rate of Ilizarov treatment for bone infections?
Studies show that Ilizarov bone transport achieves 77% excellent to good bone healing results for infected nonunion cases. When combined with proper soft tissue reconstruction, infection eradication rates can reach 96.5%.
How long does treatment take?
Treatment duration varies from 6-12 months depending on infection severity and bone defect size. This includes surgical debridement, bone transport phases, and consolidation periods.
Can bone infections recur after treatment?
With proper surgical debridement, appropriate antibiotic therapy, and complete infection eradication, recurrence rates are low. Long-term follow-up is essential to monitor for any signs of recurring infection.
Is the treatment painful?
Pain is well-managed with appropriate medications throughout treatment. Most patients experience manageable discomfort during the adjustment phases, which gradually improves as healing progresses.
What are the alternatives if conservative treatment fails?
For severe chronic infections, amputation may be considered as a last resort if limb salvage is not possible. However, advanced techniques like Ilizarov bone transport often provide limb-saving alternatives.