How We Work
Frequently Asked Questions about Bow Leg Correction
Is bow leg correction painful?
Mild discomfort is expected post-treatment, especially with surgical correction. However, pain is well-managed with medications, and most patients report it subsides within a few days to weeks.
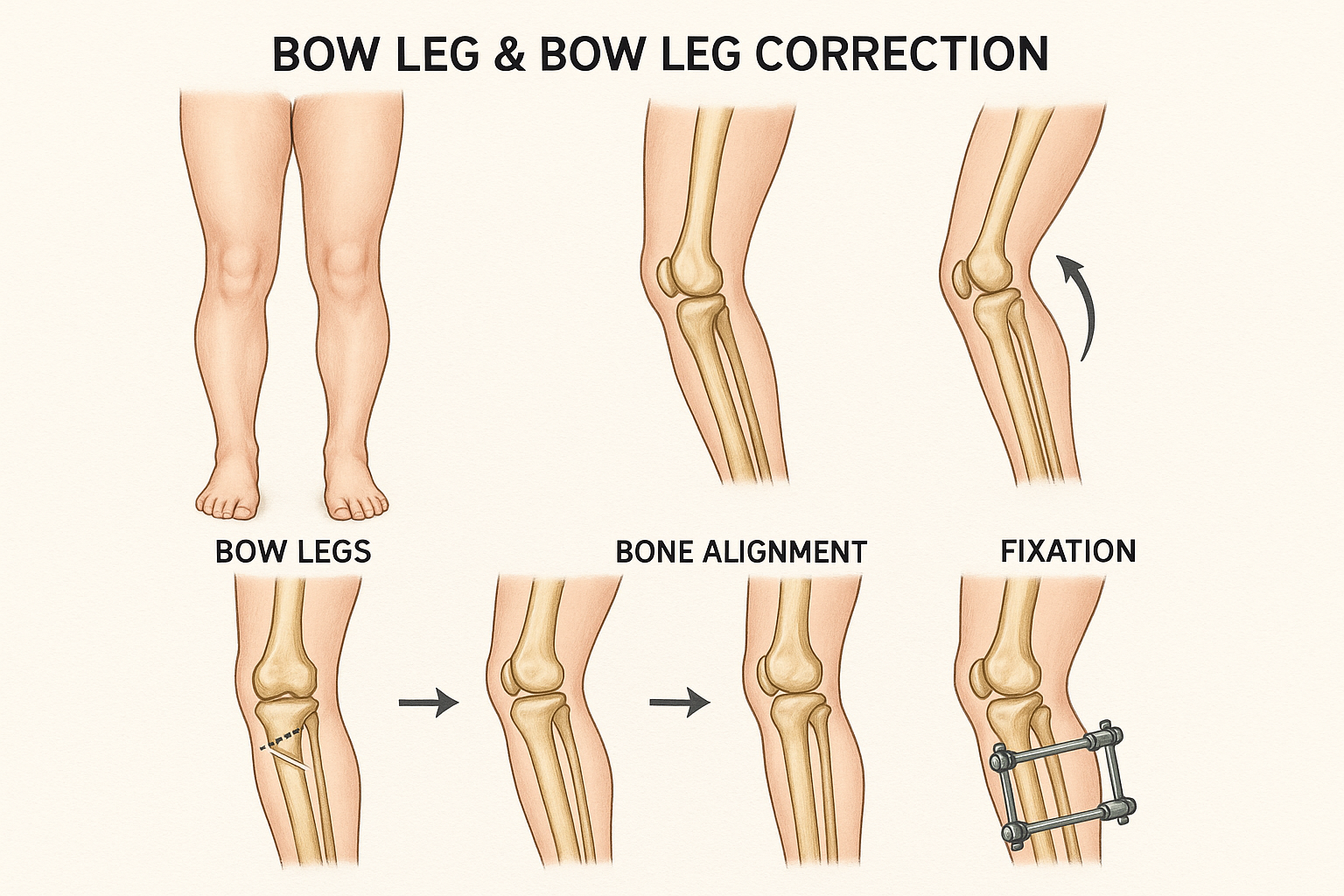
How long is the recovery after surgery?
Recovery varies by procedure. Osteotomy typically requires 3–6 months, while guided growth may take 12–18 months to fully straighten the legs. Total knee replacement recovery is around 6–12 weeks for basic mobility.
What are the chances of recurrence?
If treated correctly during growth, recurrence is rare. In adults, surgical correction offers permanent results unless underlying joint degeneration progresses due to other health factors.
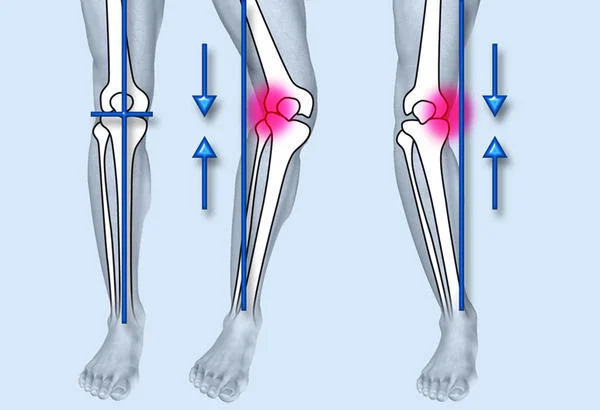
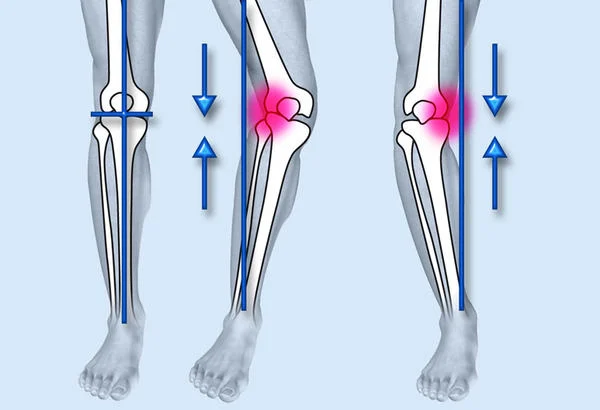
Are there non-surgical options for adults?
Non-surgical methods like physiotherapy or orthotics may help manage mild symptoms but do not correct bony deformities. Surgery is often the definitive solution for adults with moderate to severe bow legs.
Can exercise alone fix bow legs?
Exercise improves strength and mobility, but cannot realign bones once they are fully developed. It is beneficial post-correction or as preventive care in early childhood.
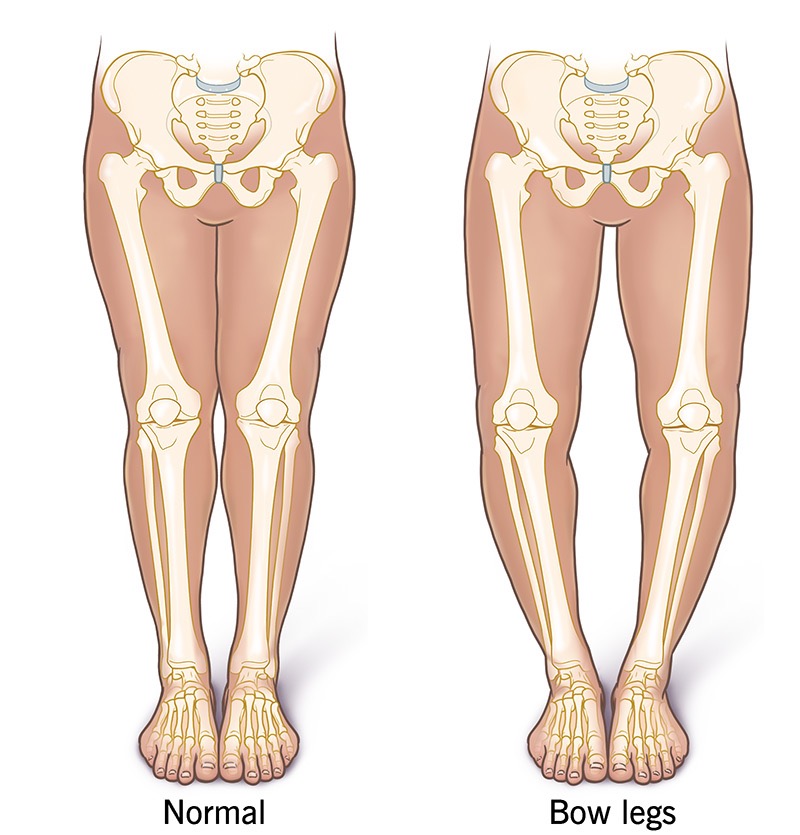
Can bow legs cause long-term complications if untreated?
Yes, untreated bow legs can lead to arthritis, gait issues, chronic pain, and deformity progression, especially in adults.
At what age is guided growth surgery most effective?
Typically between ages 4 and 11, when the growth plates are still active. Early diagnosis is key to using this minimally invasive technique.
Is bowleg correction covered by insurance?
Most insurance plans cover surgical correction when it’s medically necessary. Cosmetic procedures may not be covered unless tied to functional issues.
How soon can children return to school after surgery?
Most children can return within 2–3 weeks, depending on the procedure and their ability to move comfortably with crutches or walkers.
What lifestyle changes support better outcomes?
A nutrient-rich diet, consistent physiotherapy, avoiding high-impact activities, and maintaining a healthy weight are all vital for recovery and long-term joint health.