Frequently Asked Questions about Bone Transport
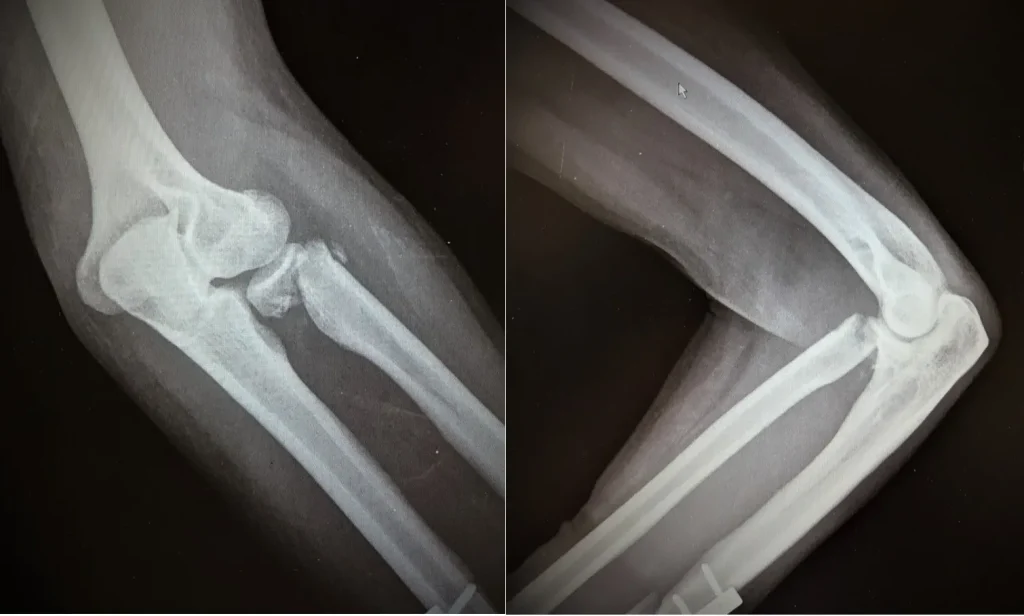
What causes a fracture not to heal (nonunion)?
Lack of blood supply, instability, infection, smoking, or chronic illness can all interfere with normal bone healing.
How long does nonunion treatment take?
Treatment may take 3 to 12 months, depending on bone type, health, and intervention used.
Is bone stimulator therapy effective?
Yes, in selected cases, especially hypertrophic nonunions or early delayed unions. It’s non-invasive and painless.
Will I need surgery for a nonunion?
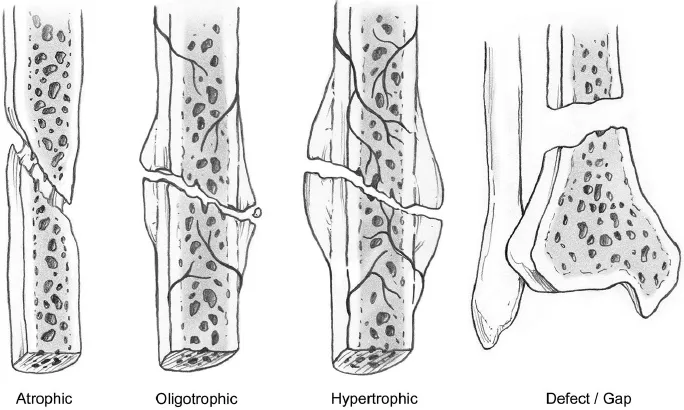
Often yes—especially for atrophic or infected nonunions—but minor cases may be managed conservatively.
Can a nonunion develop after any fracture?
Yes, especially in the tibia, humerus, and bones with poor circulation or complex fractures.
What should I expect during recovery?
You’ll go through gradual rehabilitation, physiotherapy, and regular follow-ups to monitor healing.
What are the chances of nonunion recurring?
If the root causes (like smoking or poor stabilisation) persist, there is a risk of recurrence, though it is rare under expert care.
Is nonunion painful?
Yes, it’s typically associated with persistent or intermittent pain, especially during movement.
What is the role of bone grafting?
Grafting fills gaps, supports healing, and stimulates bone regeneration where healing is biologically insufficient.
Are orthobiologics like PRP or BMPs safe?
Yes, they are FDA-approved, scientifically backed options used selectively in difficult-to-heal fractures.