Table of Contents
Introduction
Every surgery involves a healing journey – and in Ilizarov or limb reconstruction procedures, that journey can occasionally face challenges.
Ilizarov Surgery complications, such as delayed bone healing, nerve irritation, or stiffness, are not failures, but rather signs that the body or frame setup needs fine-tuning.
With timely recognition and expert intervention, nearly all these issues can be corrected without compromising the outcome.
At Dr. Divya Ahuja’s Orthopaedic & Deformity Correction Clinics in Mumbai and Thane, each patient is closely monitored using a stage-wise review protocol, allowing early identification and customized correction.
Understanding Ilizarov Healing & Why Complications Occur
The Ilizarov method relies on the body’s natural ability to form new bone (regeneration) between two segments that are gradually pulled apart.
When mechanical, biological, or patient-related factors disturb this delicate balance, complications can develop.
Common Underlying Causes
- Inadequate stability or excessive frame movement
- Poor pin site hygiene or infection
- Inconsistent distraction rate (too fast or too slow)
- Nutritional deficiencies, smoking, diabetes
- Poor compliance with physiotherapy
- Unrecognized nerve or soft-tissue tension during correction
“Most complications are correctable if caught early – the frame is flexible not only mechanically, but also in how we can adapt it to the patient.” – Dr. Divya Ahuja
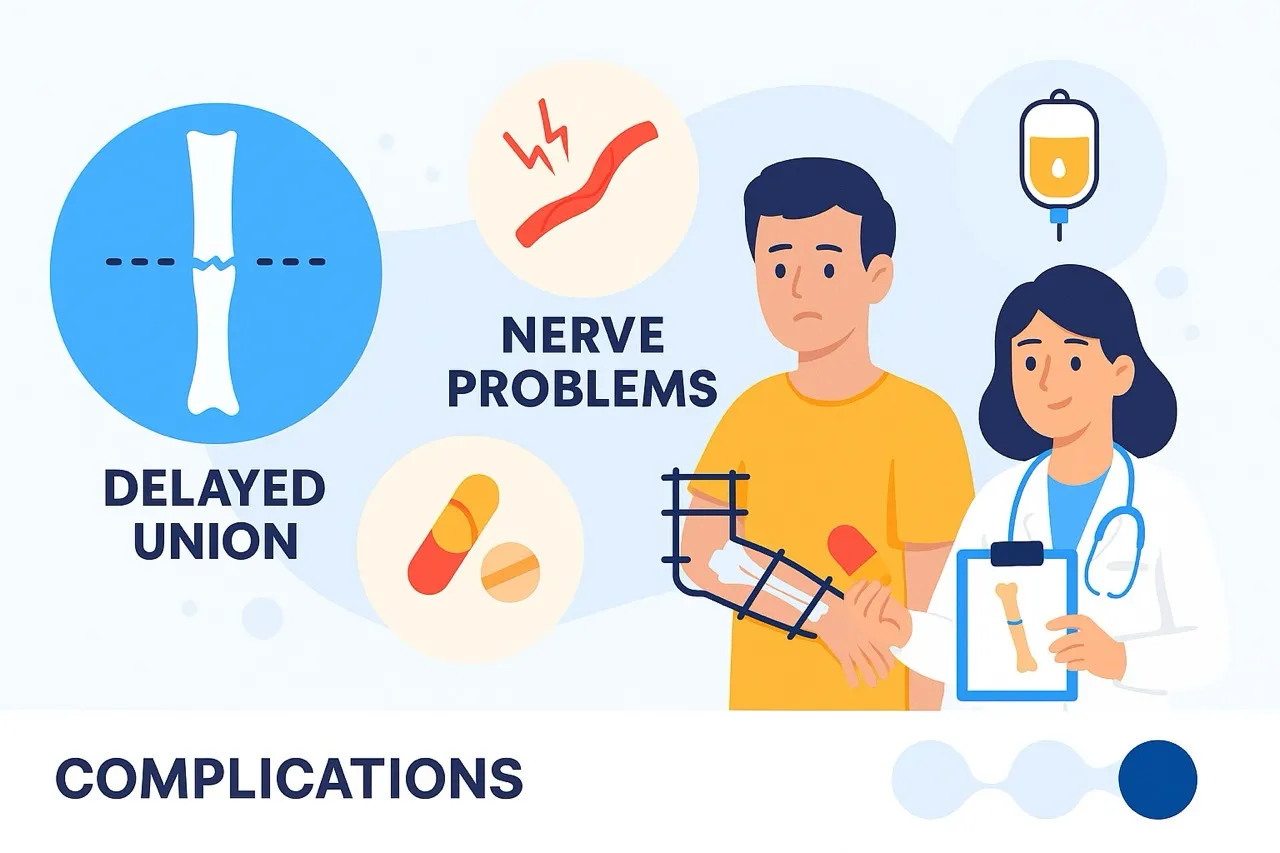
Category 1: Bone Healing Complications
Delayed Union
Definition: Slower-than-expected bone formation in the regenerate zone during consolidation.
Signs:
- Faint or patchy regeneration on X-ray
- Persistent mobility or pain at the site after the expected healing time
Possible Causes:
- Over-distraction or poor mechanical compression
- Smoking or low calcium/protein intake
- Infection reduces the blood supply
Management Strategies:
- Frame adjustment: Re-introducing slight compression to stimulate callus (“accordion technique”).
- Bone grafting: Using autograft or bone marrow concentrate if poor biological response.
- Nutrition optimization: Protein supplements, calcium, Vitamin D3, and iron support.
- Physiotherapy modification: Gradual weight bearing to stimulate bone formation.
Non-Union (Absent Bone Healing)
If the gap fails to unite even after the consolidation period:
Surgeon Adjustments:
- Re-osteotomy and re-distraction in selected cases
- Exchange nailing or internal fixation after infection control
- Bone grafting or bone transport revision
“Ilizarov allows correction even after initial non-union – it’s one of its greatest strengths.” – Dr. Divya Ahuja
Premature Consolidation
Opposite problem: Bone hardens too early before the target length is achieved.
Management:
- Stop distraction temporarily, perform re-osteotomy if needed.
- Adjust frame tension and restart gradual distraction at a slower rate.
Category 2: Neurological & Soft Tissue Complications
Nerve Stretch or Neuropraxia
Nerve symptoms — quick actions
- Pause distraction 2–3 days
- Reduce rate → 0.25 mm × 2/day
- Start B12 / methylcobalamin
- Begin gentle nerve-glide physio
- Stop distraction; inform your surgeon
- Restart later at half rate if advised
- Continue B12 / methylcobalamin
- Protect limb; avoid end-range stretch
- Urgent review if foot-drop/marked weakness
- Hold distraction until symptoms improve
- Splinting as advised; targeted physio
- Gradual return to rate per surgeon
Note: Educational only — always follow your surgeon’s protocol.
Occurs when distraction lengthens the limb faster than nerve adaptation.
Symptoms:
- Tingling, numbness, or electric-shock sensation
- Muscle weakness below the level of stretch
Surgeon’s Response:
- Pause distraction immediately for 2–3 days.
- Reduce the rate to 0.25 mm × 2/day instead of 1 mm/day
- Prescribe nerve-support vitamins (B12, methylcobalamin).
- Physiotherapy: gentle range of motion to maintain nerve glide.
Muscle Contracture or Joint Stiffness
Common near the knee and ankle due to immobilization.
Management:
- Early physiotherapy – passive and active stretching.
- Splinting at night to maintain a neutral joint position.
- Frame modification: additional hinges or elastic components for joint mobility.
- Hydrotherapy or CPM machines in the later stages.
Vascular or Circulation Problems
Excessive swelling or coldness of the toes may indicate compression of the vessels.
Handling:
- Loosen elastic bandages; elevate the limb.
- Ultrasound Doppler if needed.
- Adjust frame wires if tension compresses soft tissue.
Category 3: Infection-Related Complications
Although usually superficial, a pin site infection can delay healing and cause pain.
Preventive Approach:
- Daily pin-site cleaning with sterile technique.
- Antibiotics are based on culture in moderate infections.
- Replace loose or infected pins under local anesthesia if necessary.
Reference: See Pin Site Infections – Prevention & Management
Category 4: Mechanical & Frame-Related Complications
| Issue | Cause | Surgeon Adjustment |
| Frame loosening | Excess movement | Retighten nuts, replace wires |
| Ring deformity | Unequal tension or weight load | Realign or add connecting rods |
| Broken wire | Metal fatigue | Replace under sterile conditions |
| Skin impingement | Soft-tissue swelling | Adjust wire angle or add spacer |
Each follow-up visit includes frame inspection and X-ray to detect early mechanical issues before they cause biological delay.
Category 5: Psychological & Functional Challenges
Long treatments may affect mood, confidence, and daily life.
Dr. Ahuja’s Approach:
- Patient education and realistic expectations from Day
- Counselling, peer-support groups, and frame-friendly clothing advice
- Stepwise goals (standing, walking, cycling) to maintain motivation
“Healing is both biological and psychological – we treat the whole person, not just the bone.” – Dr. Divya Ahuja
How Surgeons Adjust & Correct Course
Dr. Divya Ahuja follows a multi-level adjustment protocol for any complication:
- Radiological Review: Assess regenerate density, frame alignment, and mechanical stability.
- Clinical Correlation: Pain, temperature, discharge, and neurovascular status.
- Frame Modification: Compression/distraction or hinge realignment.
- Adjunctive Therapies: Bone marrow aspirate, bone stimulators, or biologics when needed.
- Rehabilitation Integration: Re-balance exercises and gait training to match healing.
Pin-site care — daily checklist
Real Case Highlights
Case 1: Delayed Union – Tibial Transport
A 40-year-old patient with an infected non-union tibia showed poor regeneration.
After accordion compression cycles and local bone marrow injection, union was achieved in 3 months.
Case 2: Peroneal Nerve Irritation – Femoral Lengthening
Symptoms appeared at the 5 cm mark; distraction paused for 5 days, resumed slower. No residual weakness.
Case 3: Premature Consolidation – Pediatric Lengthening
Re-osteotomy performed, frame adjusted; complete correction achieved without functional loss.
Each case demonstrates a custom frame strategy and biologic support – hallmarks of Dr. Ahuja’s expertise.
Preventing Complications – Dr. Ahuja’s 4-P Formula
- Precision: Pre-operative planning using digital deformity analysis
- Prevention: Early physiotherapy and pin-site care education
- Promptness: Quick detection of symptoms at follow-ups
- Personalization: Adjusting distraction speed and frame design per patient
Why Choose Dr. Divya Ahuja, Mumbai’s Best Orthopaedic Surgeon for Ilizarov & Limb Reconstruction
With extensive experience in Ilizarov surgery, bone infection management, and limb deformity correction,
Dr. Divya Ahuja has successfully treated hundreds of complex cases across Mumbai and Thane.
His centres combine surgical precision with compassionate care – supported by physiotherapists, infection specialists, and modern imaging for real-time correction planning.
Key Takeaways
- Complications don’t mean failure – they’re part of personalized healing.
- Delayed or poor bone healing can often be corrected with frame adjustments.
- Nerve and soft-tissue issues resolve with timely modification.
- Close follow-up and open communication ensure the best outcomes.
- Choose an experienced Ilizarov surgeon – expertise makes the difference.
Call to Action
Facing slow bone healing or discomfort with your Ilizarov frame?
Consult Dr. Divya Ahuja, Mumbai’s trusted orthopaedic and deformity correction specialist, for expert assessment and corrective solutions.
Our Clinical Locations
Tap a location to view timings, contact, and map.
Broadway Healthcare, Dadar East
Broadway Healthcare, Dadar East
Clinic Info
- 📍 Broadway Healthcare, Dadar East, Mumbai
- 🕒 Wednesdays · 10:00 AM – 12:00 NOON
- 📞 Appointments: +91 93213 17227
Sweet Clinics, Vashi, Navi Mumbai
Sweet Clinics, Vashi, Navi Mumbai
Clinic Info
- 📍 Sweet Clinics, Vashi, Navi Mumbai
- 🕒 Fridays · 10:00 AM – 12:00 NOON
- 📞 Appointments: +91 93213 17227
Heal Well Speciality Clinic, Thane West
Heal Well Speciality Clinic, Thane West
Clinic & OPD Info
- 📍 Heal Well Speciality Clinic, Thane West
- 🕒 Every Wednesday 10:00 AM – 11:00 AM
- 📞 Appointments: +91 81691 04438
Mangal Anand Hospital, Chembur Mumbai
Mangal Anand Hospital, Chembur Mumbai
Clinic & OPD Info
- 📍 Mangal Anand Hospital, Chembur Mumbai
- 🕒 Monday, Wednesday, Friday 03-07 PM, Thursday 06-07 PM, Free OPD Saturday 02-04 PM
- 📞 Appointments: +91 70212 18182
SRV Hospitals, Tilaknagar, Chembur
SRV Hospitals, Tilaknagar, Chembur
Clinic Info
- 📍 SRV Hospitals, Tilaknagar, Chembur
- 🕒 Monday, Wednesday, Friday 11 AM-12 PM
- 📞 Appointments: +91 84518 00800
FAQs
How common are complications after Ilizarov surgery?
Minor issues like redness or stiffness are common, but major complications are rare when managed early.
What causes delayed bone healing?
Factors include over-distraction, poor nutrition, smoking, or unstable fixation.
Can a delayed union be corrected without another surgery?
Often yes – using compression cycles or bone stimulation under surgeon supervision.
What if I feel numbness or tingling in my foot?
Pause exercises and contact your surgeon immediately – early nerve adjustment prevents permanent issues.
How often should follow-up X-rays be done?
Every 3–4 weeks during distraction, then every 6 weeks in consolidation, or as advised.